Explore in-depth information on the medial condyle knee including anatomy, common injuries, diagnosis, treatment options, and recovery tips.
If you’ve been hearing about the medial condyle knee and wondering why it matters, you’re in the right place. This small but crucial part of the knee plays a major role in how your joint moves, bears weight, and responds to injury. Whether you’re a student, an athlete battling knee pain, or just curious about knee anatomy, understanding the medial condyle can unlock answers about common injuries and effective treatments. Ready to dive into what makes the medial condyle tick, why it’s vulnerable, and how to keep it healthy? Let’s get started.
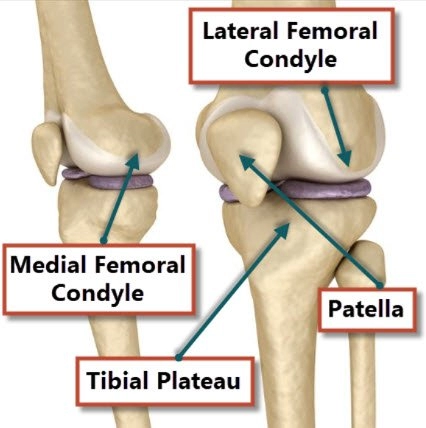
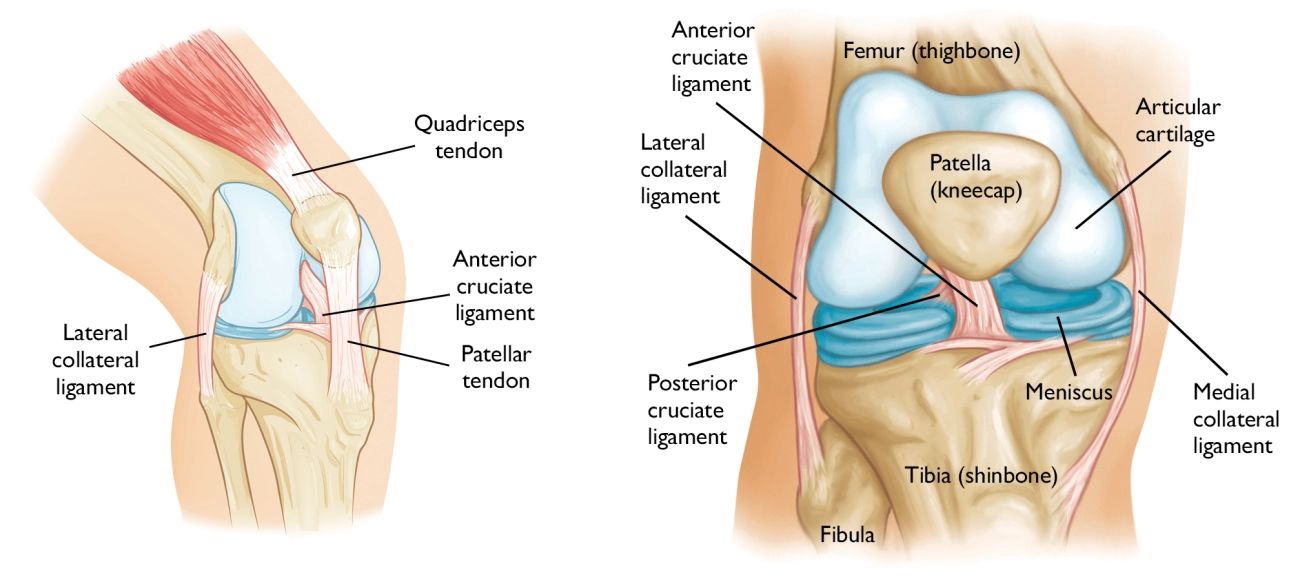
Anatomy of the Medial Condyle Knee
The medial condyle is a rounded bony prominence on the inner side of the lower end of the femur (thigh bone). It forms part of the knee joint and plays a crucial role in knee function.
Definition and Location
- The medial condyle is one of two condyles on the femur’s distal end; the other is the lateral condyle, located on the outer side of the knee.
- It sits above the tibia (shinbone) and works closely with the medial meniscus, a cartilage cushion between the femur and tibia.
- Several important ligaments, including the medial collateral ligament (MCL), attach near this area, helping stabilize the knee.
Structural Characteristics
- The medial condyle is slightly larger and more prominent than the lateral condyle.
- It has a smooth, curved surface covered with articular cartilage to reduce friction during movement.
- This cartilage allows smooth gliding against the tibia and meniscus during knee bending and straightening.
Function
- The medial condyle carries a significant portion of the body’s weight when standing and moving.
- It supports knee flexion and extension while providing stability to prevent wobbling or excessive sideways motion.
Blood Supply and Innervation
- Blood supply primarily comes from branches of the femoral and popliteal arteries, ensuring healthy bone and cartilage.
- Sensory nerves in this region help detect pain and joint position, contributing to knee proprioception and protective reflexes.
Understanding the medial condyle knee’s anatomy makes it easier to recognize how injury or disease in this area affects overall knee health and movement.
Common Medial Condyle Knee Conditions
The medial condyle of the knee is prone to several issues that can affect movement and cause pain. Here are the common problems you might encounter:
- Medial condyle fracturesThese occur from trauma like falls or sports injuries, causing a break in the bone. They often need careful treatment to heal properly.
- Osteochondritis Dissecans (OCD) of the medial condyleThis condition happens when a small piece of bone or cartilage loosens due to reduced blood flow, leading to pain and sometimes locking of the knee.
- Osteoarthritis localized to the medial condyleWear and tear can target the medial condyle, especially in people with bowed legs (varus alignment), causing cartilage breakdown and joint pain.
- Bone bruises and cartilage damageImpact injuries or repetitive stress can bruise the bone under the cartilage or damage the cartilage itself, leading to swelling and discomfort.
- Stress fractures and overuse injuriesAthletes or laborers doing repetitive knee activities can develop tiny cracks (stress fractures) or inflammation around the medial condyle, causing persistent knee pain.
Understanding these conditions can help spot issues early and get the right treatment for your medial condyle knee pain.
Causes and Risk Factors for Medial Condyle Knee Issues
Medial condyle knee problems often come from several main causes and risk factors:
- Trauma: Falls, sports injuries, and accidents can cause fractures or bruising to the medial condyle.
- Repetitive Stress: Athletes or laborers who put constant pressure on the knee, like runners, hikers, or construction workers, risk overuse injuries or stress fractures.
- Age-Related Degeneration: Osteoarthritis commonly affects the medial condyle, especially as cartilage wears down over time.
- Anatomical Variations: Conditions like varus deformity (where the knees bow outward) put uneven pressure on the medial condyle, increasing injury risk.
- Lifestyle and Local ActivitycURL Too many subrequests.
cURL Too many subrequests.
cURL Too many subrequests.
cURL Too many subrequests.
cURL Too many subrequests.
- cURL Too many subrequests. cURL Too many subrequests.
- cURL Too many subrequests. cURL Too many subrequests.
- cURL Too many subrequests. cURL Too many subrequests.
- cURL Too many subrequests. cURL Too many subrequests.
cURL Too many subrequests.
cURL Too many subrequests.
- cURL Too many subrequests.
- cURL Too many subrequests.
- cURL Too many subrequests.
- cURL Too many subrequests.
Imaging Techniques
Accurate diagnosis often needs imaging to see bone and soft tissue condition:
| Imaging Type | Purpose | Details |
|---|---|---|
| X-rays | Detect fractures and bone alignment | Good for spotting medial condyle fractures |
| MRI | Detailed view of cartilage, ligaments, meniscus, and bone bruises | Best for checking cartilage damage and soft tissue injuries around the medial condyle |
| CT Scan | Precise bone injury details | Useful when fractures are complex or unclear on X-rays |
Differentiating Medial Condyle Injuries
It’s important to distinguish medial condyle problems from:
- Lateral condyle injuries (outer knee pain)
- Meniscus tears (pain localized with clicking or locking)
Doctors use exam findings and imaging results together to pinpoint whether the medial condyle is the main issue or if another knee structure is involved.
Treatment Options for Medial Condyle Knee Issues

Non-Surgical Management
Most mild to moderate medial condyle injuries start with conservative care:
- Rest: Avoid activities that stress the knee
- Ice: Apply to reduce swelling and pain
- Compression: Use knee sleeves or wraps
- Elevation: Keep the knee raised to minimize swelling
This basic RICE approach helps control symptoms early on.
Physical Therapy
Focuses on:
- Strengthening muscles around the medial knee
- Improving knee stability and range of motion
- Correcting movement patterns to reduce stress on the medial condyle
PT is essential for both recovery and preventing future injuries.
Medications
- NSAIDs (like ibuprofen) to manage pain and inflammation
- Sometimes doctors may recommend other pain relievers if needed
Bracing and Activity Modifications
- Knee braces can offload pressure on the medial condyle
- cURL Too many subrequests.
cURL Too many subrequests.
cURL Too many subrequests.
| cURL Too many subrequests. | Purpose | cURL Too many subrequests. |
|---|---|---|
| cURL Too many subrequests. | cURL Too many subrequests. | cURL Too many subrequests. |
| cURL Too many subrequests. | cURL Too many subrequests. | cURL Too many subrequests. |
| cURL Too many subrequests. | cURL Too many subrequests. | cURL Too many subrequests. |
| cURL Too many subrequests. | cURL Too many subrequests. | cURL Too many subrequests. |
cURL Too many subrequests.
cURL Too many subrequests.
- Gradual weight-bearing and strengthening
- Range of motion exercises
- Balance and proprioception training
- Regular follow-ups and imaging for progress monitoring
Early and consistent rehab is key to restoring knee function and preventing recurrence.
Prevention and Maintenance
Preventing medial condyle knee injuries starts with a few simple but effective habits:
- Warm up and stretch properly before any physical activity. This gets the knee and surrounding muscles ready to handle stress.
- Strengthen muscles that support the medial knee, like the quadriceps, hamstrings, and hip muscles. Strong stabilizers help protect the medial condyle from strain.
- Address biomechanical issues such as poor alignment or uneven weight distribution. For example, correcting a varus deformity can reduce extra pressure on the medial condyle.
- Choose the right footwear and gear based on your local sports and activity patterns. Good shoes with proper support can lower the risk of injury, especially for runners or hikers common in many U.S. regions.
When to See a Doctor
If you experience persistent medial condyle knee pain, especially after an injury, it’s important to get checked out promptly. Here are some red flags that mean you should see a doctor right away:
- Severe swelling or bruising around the knee
- Difficulty putting weight on the leg or inability to walk
- Sudden instability or the knee giving way
- Limited range of motion that doesn’t improve with rest
- Sharp or worsening pain in the medial condyle area
Early diagnosis is crucial to prevent further damage to the knee’s structures like cartilage and ligaments. The medial condyle plays a key role in weight bearing, so untreated injuries can lead to long-term problems such as osteoarthritis or chronic pain.
At Vast, we specialize in knee anatomy and injury management. Our team uses advanced imaging techniques and thorough physical exams to accurately diagnose medial condyle issues. From conservative treatments to surgery, we guide you through all options to help you recover and maintain a strong, healthy knee.
FAQs about Medial Condyle Knee Injuries
What exactly happens when the medial condyle is injured?
When the medial condyle is injured, it usually involves damage to the bone, cartilage, or nearby ligaments. This can lead to pain on the inside of the knee, swelling, and trouble moving the joint. Injuries range from fractures and bone bruises to cartilage tears, all affecting how the knee bears weight and moves.
Can medial condyle injuries heal on their own?
Some minor injuries, like small bone bruises or mild cartilage irritation, may improve with rest and physical therapy. However, more serious conditions like fractures or osteochondritis dissecans typically require medical treatment. Ignoring symptoms can lead to worsening damage, so it’s best to get evaluated early.
How long is the recovery time after medial condyle surgery?
Recovery depends on the injury and surgery type. For example:
- Arthroscopic procedures might take 6 to 12 weeks for basic healing.
- Fixation of fractures can require 3 to 6 months, including rehab.
- Cartilage repair techniques, like microfracture or OATS, may need 4 to 9 months before full activity.
Physical therapy is key throughout recovery to rebuild strength and knee function.
Are medial condyle injuries more common in certain populations or sports?
Yes. Athletes in high-impact sports like football, basketball, and soccer are more prone to medial condyle fractures and cartilage injuries. Older adults often develop osteoarthritis concentrated in the medial condyle due to wear and tear. People with knee alignment issues like varus deformity also have a higher risk of medial condyle wear.
How is osteoarthritis diagnosed specifically in the medial condyle?
Doctors use a combination of clinical exams and imaging. X-rays show joint space narrowing, bone spurs, and changes focused on the medial condyle. MRI scans provide a detailed look at cartilage damage and bone changes in that area. Diagnosis helps guide treatment focused on relieving pain and improving knee function.